For a food bank or pantry, getting into Food is Medicine often raises more questions than answers.
Should an organization embrace produce prescriptions, healthy food boxes, or medically tailored meals, to name a few options? What is the best way to work with the managed care organizations that pay for it all? How exactly will they pay for it? What does state policy allow?
Those high-level questions don’t begin to address the many technical challenges of trying to bridge the hunger relief sector and the healthcare sector. “This is like a startup environment,” said R.J. Briscione, Principal at Health Management Associates, speaking at a recent webinar sponsored by the Medicaid Food Security Network (MFSN). “You have to have a startup mentality for this.”
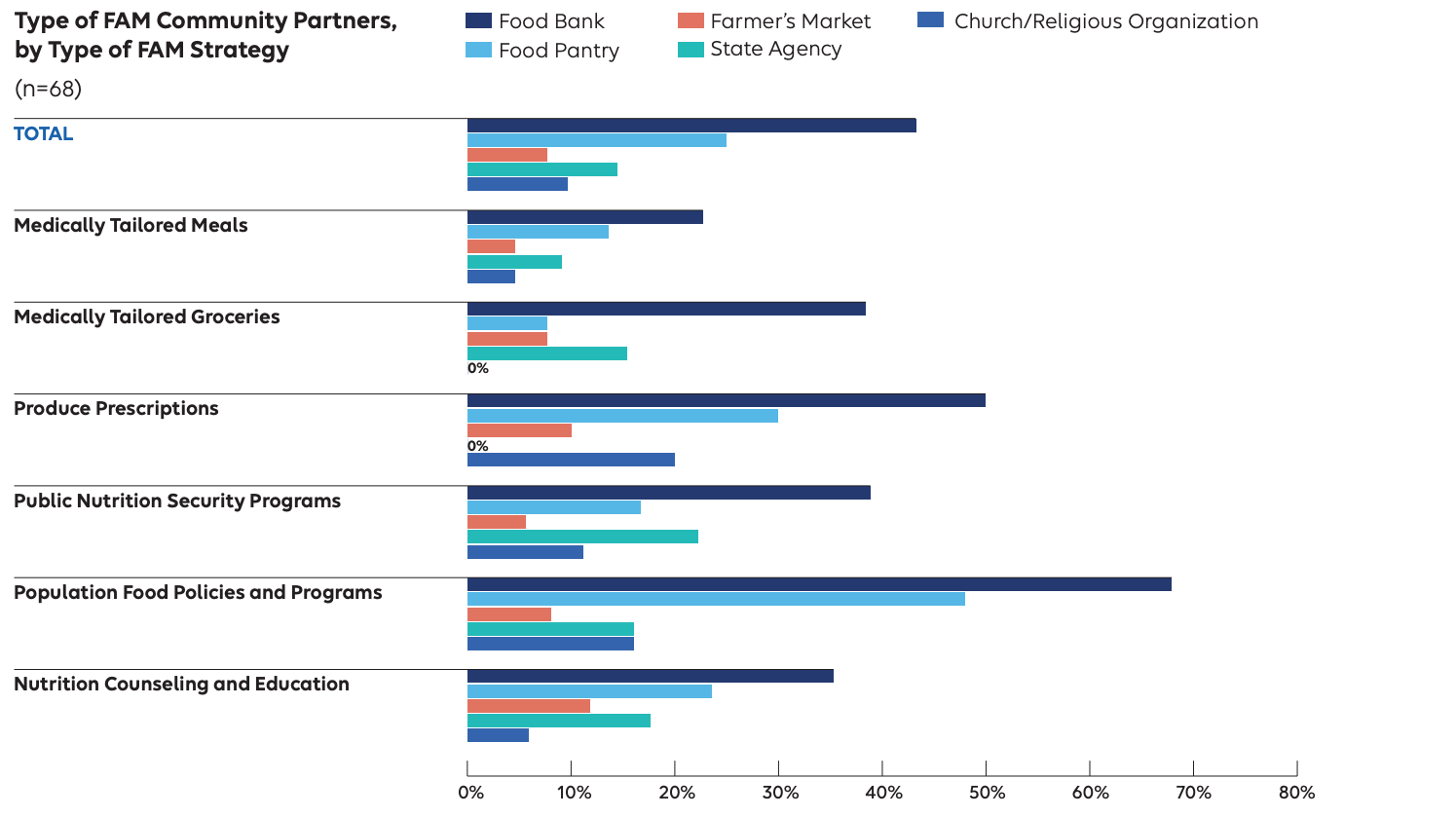
Despite mostly being well past the startup stage, many community based organizations are playing a solid role in Food is Medicine initiatives. Nearly half of Food is Medicine programs surveyed have a community-based organization as a partner, with the most common partners being a food bank, followed by a food pantry, according to a report released earlier this month from Elevance Health Public Policy Institute, a unit of Elevance Health (see chart, above).
“Community partnerships are integral in the delivery of Food is Medicine,” noted the report.
The report, which surveyed the Food is Medicine initiatives happening within Elevance’s affiliated health plans, described the most common types of Food is Medicine interventions as those that aim to broadly promote access to nutritious food through public programs like SNAP or WIC (71%). Half are focused on more intensive treatments like medically tailored meals and groceries, or produce prescriptions. In terms of population focus, Food is Medicine programs are most likely to address people with diabetes.
Slowly but surely, progress is being made on working out some of the kinks that have impeded the advance of Food is Medicine. A San Francisco company called Fullwell, for example, is smoothing out differences in medical billing codes that make it difficult to communicate broadly about treatments and outcomes in Food is Medicine interventions.
As Katie Ettman, Deputy Director at Fullwell, explained on the MFSN webinar, “While we have lots of states that are working to integrate food into healthcare, in many instances we’re not using a shared language. So we can’t fully communicate to the healthcare system the value add of the services we have.”
The terminology adopted by states makes it difficult to compare interventions, she said, noting that Food is Medicine initiatives in Massachusetts refer to “nutritionally appropriate food boxes,” while those in Michigan specify a “healthy food pack.” New Jersey, Washington, Oregon and Illinois use the term “pantry stocking,” while D.C. refers to “protein boxes.” The Fullwell project is aimed at bringing together experts from across the country to devise medical codes that would define the full spectrum of Food is Medicine interventions.
Said Ettman, “Hopefully, in the coming months and years, we will have new ways to embed these services into our healthcare system and billing system.”
In another Food is Medicine advance, the Food is Medicine Coalition announced earlier this month that it has introduced a membership program for organizations that provide medically tailored groceries. Often, those organizations are food banks or pantries. The new program adds to FIMC’s existing membership program for medically tailored meals, and offers access to services like technical assistance, research opportunities, and communities of practice. – C.C.
Like what you’re reading?
Support Food Bank News