A new survey from Food Research and Action Center points to the need for much greater communication between healthcare centers and hunger relief organizations when it comes to food insecurity screening and intervening.
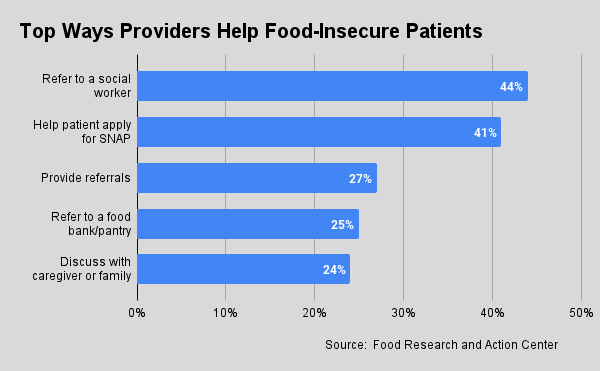
Only 25% of healthcare providers refer their food-insecure patients to a food bank or pantry for food aid, according to the survey, which polled 144 healthcare providers regarding their interactions with patients aged 50 years or older.
Healthcare providers can be a valuable resource for identifying cases of food insecurity, since many of the diseases their patients suffer from stem from poor nutrition. Virtually all of the survey respondents (99%) agreed or strongly agreed that screening for food insecurity in a clinical setting is important.
While the majority (88%) screen all or some of their patients for food insecurity, far fewer have interventions in place to address food insecurity once it’s discovered (see chart above). Their most common responses are to refer food-insecure patients to a social worker (44%), help them apply for SNAP (41%), or provide referrals (27%). Referring patients to a food bank or pantry was the fourth-most common intervention (see the 25% mentioned above).
“The ability to carry out effective referrals on an ongoing basis are challenged in different healthcare organizations,” affirmed Joe Arthur, CEO of Central Pennsylvania Food Bank, which has been working with at least 20 healthcare partners and federally qualified healthcare centers in the food bank’s 27-county service area for the past eight years.
Over the years, the food bank has moved from small-scale, grant-funded food as medicine projects into more strategic agreements with providers that involve everything from basic screening and referrals, to tailored food boxes, to distributions at on-site health-center pantries. Referrals, in particular, suffer from widespread issues such as staffing challenges and the difficulty of doing follow-up to ensure referrals were acted upon, Arthur said.
Smooth referral processes will become even more important as the healthcare industry responds to a stipulation from the Centers for Medicare and Medicaid Services that all hospitals and clinics in federal payment programs screen their patients for social determinants of health, including food insecurity. The ruling is sure to result in the detection of many more food-insecure households. (See how some food banks are responding here.)
Healthcare providers most often execute referrals by providing information on food resources via a paper hand-out (41%) or verbally (35%), according to the FRAC survey. Walking patients to an on-site pantry (31%) or making notes in electronic medical records (28%) happen with less frequency.
At Central Pennsylvania Food Bank, two SNAP outreach team members funded by two different healthcare partners currently receive referrals of food-insecure patients from those centers. One partner is particularly effective at executing the referrals, pointing to the importance of each individual healthcare center’s procedures. “How you set up the referral processes and operations really, really matters,” Arthur said, adding, “We’re working intensively to get the challenges in front of the decision-makers who can actually make some changes.”
 About five years ago, the food bank hired a Health Innovations Manager to oversee the food bank’s healthcare partnerships. Initially, the position reported directly to Arthur, to “give it the weight that it needed in our organization to get things done,” Arthur said. Now, the position is integrated with the team that supports all of the food bank’s partner agencies.
About five years ago, the food bank hired a Health Innovations Manager to oversee the food bank’s healthcare partnerships. Initially, the position reported directly to Arthur, to “give it the weight that it needed in our organization to get things done,” Arthur said. Now, the position is integrated with the team that supports all of the food bank’s partner agencies.
Often, healthcare centers don’t know if a patient has followed up on a food-bank or other type of referral. According to the FRAC survey, nearly one-third (32%) said patients tell them whether they followed up on a referral, while 23% said they often don’t know what happens with referrals, and 20% said they need help closing the referral loop.
Healthcare providers see the anti-hunger community as an important partner. When asked about support needed to better address food insecurity among patients, 45% cited funding for hunger relief organizations to help patients connect to resources. The only support ranked higher was training for healthcare professionals on how to connect patients to resources like SNAP and food (62%).
Despite the rise of tools like Medicaid 1115 waivers and produce-prescription programs, these interventions are among the least likely ways healthcare providers are currently seeking to help their food-insecure patients (see chart, above left).
Proving the efficacy of healthy food for food-insecure patients continues to be a challenge and is an area where Central Pennsylvania Food Bank is paying extra attention. Rather than chasing one-off grants, it is looking to work with major strategic programs at the federal or state level that are committed to food as medicine endeavors. “We’ve got to get strategic about it,” Arthur said. “That requires solid agreements, reporting efficacy and getting paid for the work.” – Chris Costanzo
Like what you’re reading?
Support Food Bank News