A recently published paper in the Journal of the American Medical Association gives the cold shoulder to the concept of Food is Medicine.
The authors, affiliated with Johns Hopkins University and the University of Pennsylvania, describe all the attention being paid to Food is Medicine – including by the White House at its conference on hunger, health and nutrition last year – as “unjustified” by Food is Medicine’s likely benefit.
The authors make the case that getting people to eat healthfully, even if they are being provided food by their healthcare provider, is just difficult to do. For starters, the healthcare system is overburdened, difficult to access, and does not have a good track record of being able to coordinate with other providers, such as nutrition counselors, they say.
Perhaps most important, patient behavior when it comes to healthy eating, is difficult to influence. Patients already exhibit low compliance when it comes to taking medications. Eating healthfully, meanwhile, requires a lot more effort, with less direct impact on outcomes. “We are thus skeptical that food is medicine programs will lead to long-term improvements in diet or health,” the authors wrote.
It would be better to put resources into public-health efforts like taxing unhealthy food and improving nutrition labeling. Even better would be to modernize existing government programs like SNAP or WIC, which already exist to provide food to families in need. Rather than give out food prescriptions at health care visits, why not provide additional fruits and vegetables through SNAP, the authors say.
Certainly, there is already widespread support among Food is Medicine advocates to strengthen existing government programs to promote better public health. Caree Jackson Cotwright, Director of Nutrition Security and Health Equity at the USDA, speaking at the Food is Medicine Policy Summit in D.C. in November, noted that WIC is actually a nutrition prescription program, even though people don’t think of it that way.
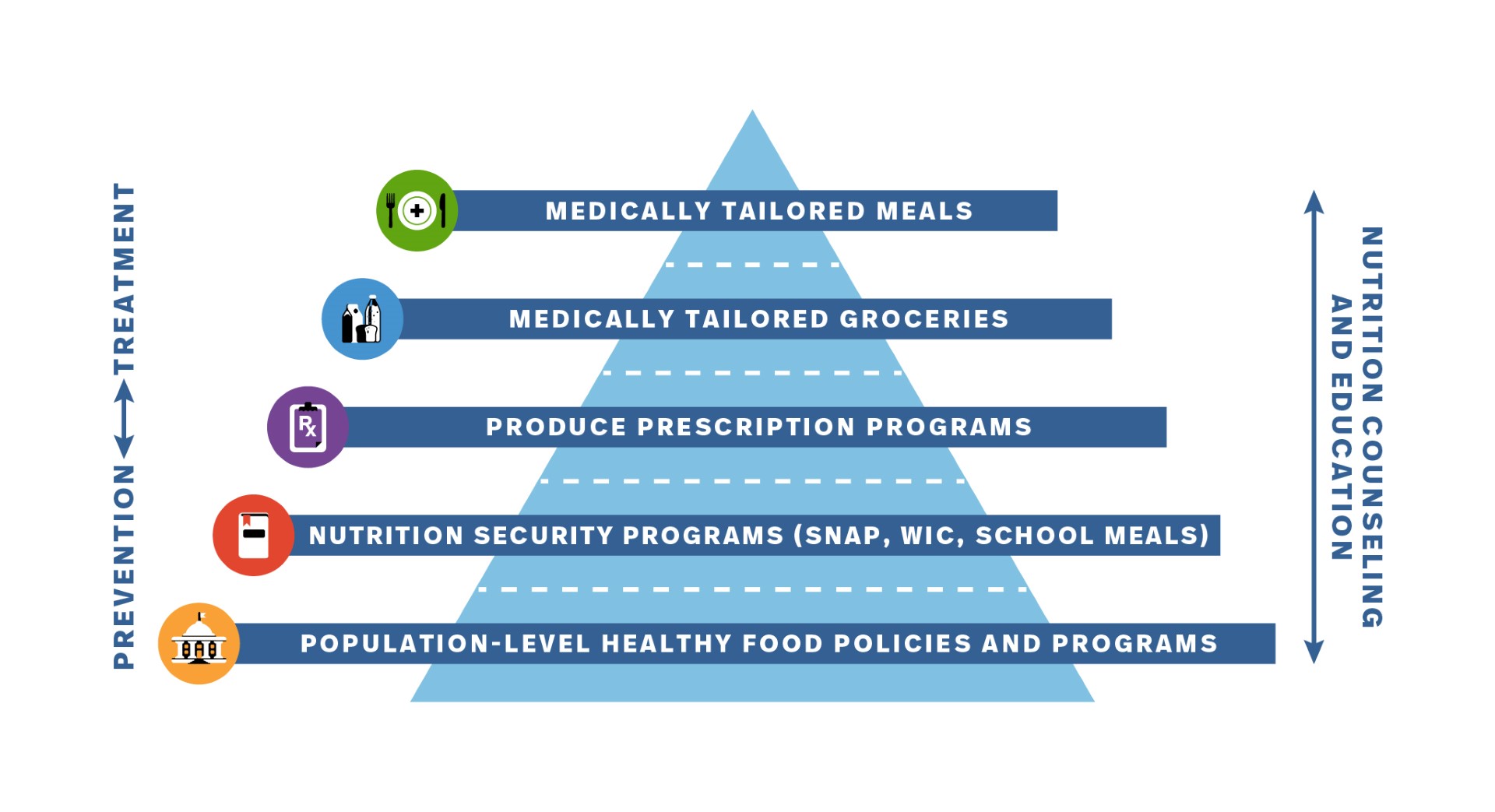
Dr. Kofi Essel, Director of Food as Medicine at Elevance Health, pointed to the Food is Medicine pyramid (see top) to underscore that healthy food policies and programs, along with nutrition assistance programs like SNAP and WIC, form the basis of the Food is Medicine approach. The top three portions of the pyramid – produce prescription programs, and medically tailored meals and groceries – are what many people think of as Food is Medicine, but “are just part of the puzzle,” Dr. Essel said.
Elevance is seeking to address the foundational aspects of Food is Medicine by improving programs like SNAP, and also working with community based organizations like food banks and pantries “as a strategic part of moving the needle on improving the health of our members and communities around the country,” he said.
The Food is Medicine movement still will have to counter naysayers, especially as mainstream food companies like Amazon, Kroger and Instacart, as well as a wave of new private food companies, develop related products. Food is Medicine “is a boon to the food industry,” noted the JAMA study’s authors.
Food policy analyst Marion Nestle agreed in a recent post that the food industry is a main beneficiary of Food is Medicine. “Count me as an FIM skeptic,” she wrote. “It is not likely to scale up enough to address chronic disease in any significant way.” – Chris Costanzo
Like what you’re reading?
Support Food Bank News
This article was made possible by the readers who support Food Bank News, a national, editorially independent, nonprofit media organization. Food Bank News is not funded by any government agencies, nor is it part of a larger association or corporation. Your support helps ensure our continued solutions-oriented coverage of best practices in hunger relief. Thank you!
Connect with Us: