In theory, healthcare and hunger-relief entities are excellent partners in serving food-insecure people in their communities. In reality, there are often barriers to making those partnerships click.
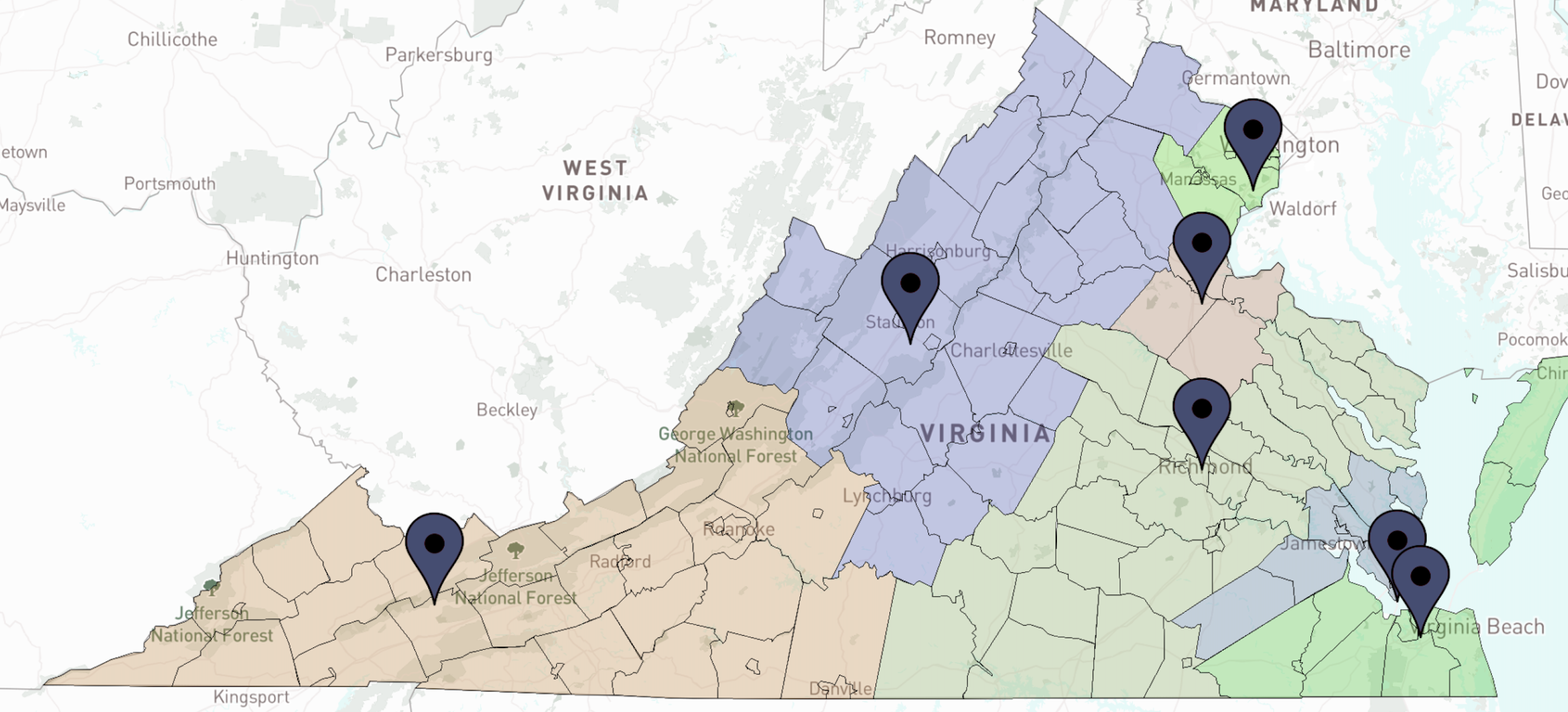
The Federation of Virginia Food Banks and the state’s seven member food banks are working to break down those barriers with a three-year plan that aims to deepen food bank/healthcare partnerships. The effort is novel in elevating the activity to the state level, an approach that better suits the needs of statewide hospital networks and insurance companies.

“So much of this work originated as separate pilot programs and we said, ‘That’s not doing enough. It’s not making the difference that we need it to,’” said Meaghan Butler, Health Equity Director at the Federation. “To really do this successfully, we need to envision our entire service delivery area as having a role in health.”
Sentara Healthcare, a large nonprofit hospital network in the state, helped bring the need to light when it began making investments in food security as part of its social responsibility plan. To avoid having to strike up relationships with seven different food banks, it approached the Federation. “Sentara saw the potential of working through the Federation very early on, because of its larger footprint,” Butler said. In addition, a total of $1 million in grants from Feeding America’s Boundless Collaboration program, including $200,000 for planning and $800,000 for implementation, helped propel the project.
So what is the Federation doing to promote partnerships between hunger relief and healthcare? For one, it established a standard definition of what it means to be a “healthy” food pantry. That’s helpful for healthcare partners that previously didn’t know what their patients could expect from pantries labeled “healthy.”
Now Virginia has a statewide Healthy Pantry Model that describes 20 or so practices that pantries can follow to better support the health of their communities. The guidelines were established by a design team consisting of ten healthcare entities, two community partners, 21 local food pantries, 11 food bank staff members, and a cohort of 27 neighbors facing food insecurity. “We made sure that neighbors were really driving this process,” Butler said.
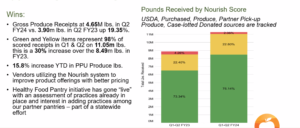
For neighbors, the number-one requirement for a healthy pantry is fresh produce, the Federation found. Healthcare providers meanwhile specified that patients should be able to easily access the pantry, whether through weekend hours, after-hours availability, online ordering or home delivery. Other requirements that emerged included having familiar, culturally relevant food and dietary options like low sodium.
Now the Federation is embarking upon a yearlong process of getting the state’s pantries to assess their current practices and take advantage of various resources and grants to move toward the common standard. A survey of neighbors will help to gauge the impact of the work.

Another big initiative is to have a standard communications tool to support the process of referring food-insecure healthcare patients to hunger relief organizations. The Federation was aided in this effort by an earlier decision by the Virginia Department of Health to rally around the Unite Us communications tool. Through Unite Us, healthcare providers can execute referrals to food assistance in a way that complies with patient privacy (or HIPAA) regulations. “It certainly made it easier from our perspective that we didn’t have to choose between competing platforms,” Butler noted.
The next step of the process is to connect referred patients to community partners that can provide wraparound services. Recently, the Virginia Department of Health awarded $175,000 of funding to help food banks hire referral coordinators to help in this process. “We’re still determining the best workflows to enable these partnerships to thrive,” Butler said.
The Unite Us platform also could eventually serve as a mechanism for food banks to get reimbursed by insurance providers for providing nutritious food to food-insecure people. As momentum around Medicaid 1115 waivers continues to grow, the Federation is making decisions about Unite Us with a Medicaid reimbursement pathway in mind, Butler acknowledged.
Eddie Oliver, Executive Director of the Federation, summed up the value of addressing hunger relief and healthcare partnerships at the state level. “It just makes a ton of sense to collaborate,” he said. “The hospital networks are demanding it. The insurance companies are demanding it. Whether you’re pursuing an 1115 waiver or funneling federal grant money, that connection point with the state government is really critical.” – Chris Costanzo
Like what you’re reading?
Support Food Bank News