There are plenty of opportunities to go around in Food as Medicine, and celebrity chef Michel Nischan aptly summed them up last week at the Food as Medicine Policy Summit held in Washington D.C.
Patients get food to improve their lives; doctors get tools to slow devastating disease; insurance plans get savings, and the food system gets new things to sell. “It’s kind of like we have this multibillion-dollar miracle drug that hasn’t been released yet,” he said.
Nischan has good instincts when it comes to sensing opportunity, having already helped figure out a way to permanently tap USDA funding to support produce prescriptions (see our article here). The possibilities presented by harnessing insurance funding for Food as Medicine are even bigger. “It’s impossible to overstate the opportunity,” he said.
Indeed, there was a buzz to the sold-out conference not typically in evidence at a standard policy affair. Speakers included plenty of policy people, as well as representatives from retail grocers, health insurers, providers of consumer data, and entrepreneurial tech companies.
What about the role of the hunger-relief sector in the emerging Food as Medicine ecosystem?
Ipyana Spencer, Chief Health Officer at Meals on Wheels America (pictured above), noted the work that her organization does around the country in close coordination with healthcare plans like Medicare Advantage, helping health plans identify and coordinate benefits, often related to providing meals to patients once they’ve been discharged from the hospital.
Beyond basic food delivery, Meals on Wheels America offers the added advantage of visiting and seeing patients in their home environments. “We are the eyes and ears for a lot of what goes on in individuals’ lives,” Spencer said. Being on the ground helps ensure a plan’s benefits are not only accessible, but utilized. Providing a cart to take to the grocery store, for example, is not a helpful benefit for a patient in a wheelchair, she noted.
Organizations like Meals on Wheels also have insights into communities they serve, such as whether there are enough grocery stores nearby. And the ways in which culture, religion or ethnicity may be affecting how people manage their diseases. All of that can help the healthcare sector better target their services to specific populations. Spencer told insurers: “You need community-based organizations. You need people on the front lines.”
Alissa Wassung, Executive Director of the Food is Medicine Coalition, seconded that notion. The Food is Medicine Coalition champions medically tailored meals through advocacy and research, and also trains an annual cohort of organizations, usually made up of food banks, on building capacity to offer the meals. “We don’t believe any intervention will be successful without the community involved,” Wassung said.
Aside from community involvement, sustainable funding of Food as Medicine through insurance emerged as a big concern. “Right now, we don’t have a widespread coverage mandate for Food as Medicine services,” said Rachel Landauer, Clinical Instructor at the Center for Health Law and Policy Innovation at Harvard Law School. While Medicaid 1115 waivers hold the promise of public insurance paying for nutrition services, only six states currently offer such waivers (for more on 1115 waivers, see our article here).
Massachusetts is one of those states, and Revere Food Pantry, which distributes only plant-based food from within Massachusetts General Hospital, relies mostly on Medicaid dollars to fund the food it distributes, said Dr. Jacob Mirsky, Medical Director at the hospital and Founder of the pantry. “What we are not getting for our patients is funding care from private insurers,” he said, a situation that worries him.
Insurers cover medications (such as the weight-loss drug Ozempic), as long as the drugs are shown to be safe and effective, he noted. More large randomized, controlled trials are needed to demonstrate the same for plant-based diets. “The future for Food as Medicine, especially in terms of the provision of food, is to think about how we are going to get anywhere near the low bar that’s available right now for coverage of medications, especially given the fact that there is limited research funding to demonstrate that” for Food as Medicine, he said.
Organizations are doing what they can to get funding to come their way. Capital Area Food Bank is embracing research as it seeks to get sustained funding from insurers through a Medicaid 1115 waiver. Since early 2022, it has been operating a food pharmacy at Children’s National Hospital, where more than 60% of the kids being treated are food-insecure. Patients and their families get roughly 35 pounds of healthy food to take home after each doctor visit.
Now, Capital Area is taking the initiative further. “We knew we had to dig deeper and have a more evidence-based approach to be able to be prepared for an 1115 waiver,” said Susan Topping, Senior Director of Food, Policy and Impact. So the food bank is moving forward with a 400-person research study, in which half of the cohort will have healthy meals delivered to their homes, with their health outcomes tracked for 18 months.
The food bank is working with Hungry Harvest so families can order from an online menu of culturally appropriate food that is supportive of diabetes care. The pilot will track clinical outcomes like blood glucose levels and liver function, as well as behavioral outcomes like depression, knowledge around nutrition, and overall dietary consumption. It will also compare healthcare utilization and costs between the two groups. The long-term goal is to evolve the food pharmacy from a pilot to a “new standard of care,” Topping said.
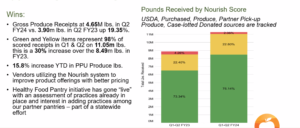
DC Greens, an advocacy and community service organization, is also preparing to attract insurance funding, having revamped its produce prescription program from one that was difficult to access and navigate, to one that is now much more highly utilized, thanks to new technology. Fresh Connect technology from Boston-based About Fresh is making it possible for families to have their monthly prescription funds automatically loaded onto benefit cards and to use the cards at many more grocery stores than before (see more on Fresh Connect in our article here).
DC Greens’ timing is good because Washington D.C. just announced it would renew its Medicaid 1115 waiver. “If we’re advocating for reimbursement in our 1115 waiver, we need a program model that is set and ready to go,” said Kristin Sukys, Health Policy Specialist. Its new produce prescription program gives it the data it needs to prove impact and utilization, as well as a scalable model “that’s more appealing for Medicaid reimbursement,” she said.
Optimism for the future of Food is Medicine was especially strong among the entrepreneurs in the room. Josh Hix, Co-founder and CEO of Season Health, which partners with health insurance plans so they can offer dietician-supported nutrition counseling to members with diet-related disease, called the Food as Medicine movement complicated from a policy perspective, but exciting because “technology can obscure that.” Season Health lets users tap into nutrition services that are paid for by their insurer, without them being aware of the complexity behind that delivery system. “It works,” Hix said. “It works really well.” – Chris Costanzo
Like what you’re reading?
Support Food Bank News
This article was made possible by the readers who support Food Bank News, a national, editorially independent, nonprofit media organization. Food Bank News is not funded by any government agencies, nor is it part of a larger association or corporation. Your support helps ensure our continued solutions-oriented coverage of best practices in hunger relief. Thank you!
Connect with Us: