Of the ten recommendations that the Bipartisan Policy Center recently issued for advancing Food is Medicine, only one addresses the role of community based organizations (CBOs) that provide food and nutrition (i.e., food banks and pantries).
The Food is Medicine movement is gaining prominence as a way to address spiraling health care costs related to poor diet and nutrition, and engaging CBOs in the effort is “crucial for its effectiveness,” the Center said. To that end, its eighth recommendation calls for the sharing of best practices to help CBOs exchange data with health care providers in a way that meets patient-privacy requirements.
Data exchange is no small task (as Food Bank News has written about here.) Current laws related to keeping patient data private represent a new and complicated regulatory landscape for CBOs, and the uncertainty, cost and complexity of it all can be “a large enough barrier to prevent collaboration between CBOs and health care systems” from happening in the first place, the report said.
While one of the main goals of Food is Medicine is to foster insurance coverage for nutritious food, both public and private insurers currently offer limited coverage for Food is Medicine efforts, the report noted. That’s despite a recent study that found medically tailored meals could prevent 1.6 million hospitalizations and save $13.6 billion in healthcare costs each year.
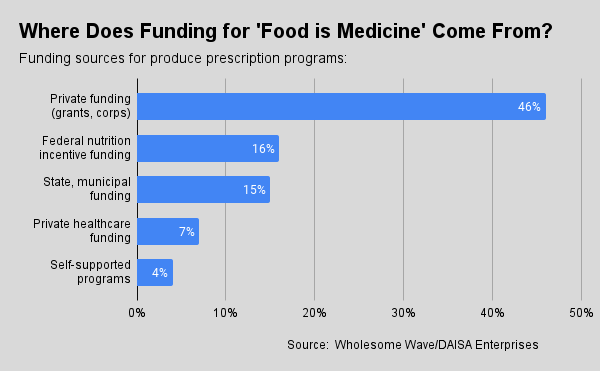
To date, funding for Food is Medicine efforts, specifically produce prescriptions, is mostly through private sources (46%), such as foundations and corporations, according to the report, citing research commissioned by Wholesome Wave, a provider of produce prescription programs. Another 16% of funding comes through federal nutrition incentives, while 15% comes from state, municipal and other local funding. Seven percent of funding is from private healthcare, while 4% of organizations support produce prescription programs through their own budgets (see chart above).
The report highlighted two examples of private sector companies that are investing in Food is Medicine interventions, both of which are working extensively with food banks. Instacart, for example, introduced online SNAP in all 50 states, among other innovations, and has a program called Community Carts that lets people use an app to donate nutritious groceries to more than 100 Feeding America food banks.
Meanwhile, the philanthropic arm of Elevance Health, formerly known as Anthem, Inc., is awarding more than $14 million to Feeding America through 2025 to foster partnerships between food banks and healthcare providers. This investment builds upon two previous rounds of funding and seeks to support better data collection, sharing and analysis between food banks and healthcare providers.
The report from the Bipartisan Policy Center, which was formed 16 years ago by two Democratic and two Republican senators to foster bipartisan solutions, came out of its Food is Medicine working group, convened in March. Among the 14 members of the working group there are grocers, insurers and doctors, but no representatives from CBOs.
The same week that the Center issued its report, the Centers for Medicare and Medicaid Services released a bulletin clarifying a few things around Food is Medicine, including ways to provide it to an entire household, not just one individual, and how to renew a six-month provision of Food is Medicine for another six months. In a post on LinkedIn, Dariush Mozzafarian, Director of the Tufts Food is Medicine Institute, who is also a member of the Bipartisan Policy Center’s Food is Medicine working group, lauded the “vision and thoughtfulness” of the updates. – C.C.
Like what you’re reading?
Support Food Bank News