Feed More of Virginia recently disclosed the results of a Food is Medicine pilot that delivered significant improvements in health outcomes.
The low-cost pilot resulted in an average decrease in blood sugar levels of nearly ten percent and notable improvements in blood pressure among participants, while also decreasing food insecurity by more than 50%. Now Feed More is exploring more ambitious healthcare partnerships.
The activity puts Feed More among a growing number of food banks, such as Food Bank of Central and Eastern North Carolina and Second Harvest Food Bank Santa Cruz County and Tarrant Area Food Bank, seeking to participate in the burgeoning Food is Medicine movement. As the healthcare industry increasingly recognizes the value of nutritious food in promoting health, it is calling upon hunger relief agencies to act as partners in sourcing and distributing that food.
Ongoing collaboration between the healthcare and hunger relief sectors seems likely, as the Food is Medicine movement continues to expand. “I see healthcare partnerships just woven into the fabric of where food banks are,” said Allison Hallberg, Health Initiatives Director at Feed More.
Hallberg arrived at Feed More just over two and a half years ago to head up the Health Initiatives Department, the food bank’s newest unit. At the time, the food bank had a relationship with one healthcare provider, which had come about in partnership with Elevance Health Foundation. (Feed More is one of a group of about 20 Feeding America food banks that are working with Elevance, as the insurer seeks to increase the capacity of food banks to partner with healthcare through a $14 million+ investment.)
The Elevance relationship helped Feed More expand into ten healthcare partnerships across 25 sites, now supported by five full-time staff. The just-completed pilot occurred outside of the Elevance grant relationship. “We learned so much,” Hallberg said, “including interacting with a healthcare insurance company as a funder. It was a truly valuable experience.”
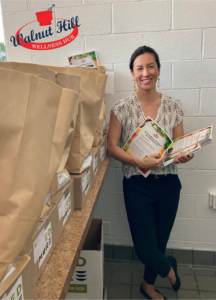
The beginnings of the pilot trace back to Feed More’s desire to more proactively address Petersburg, a city near Richmond, Va., that it had identified as a priority due to its high rate of food insecurity and poor health outcomes. Feed More then began talking with United Healthcare, a Medicaid insurance provider, and Walnut Hill Pharmacy, which had purchased a building that previously housed a Pizza Hut and then a Jamaican fast food restaurant. The pharmacy wanted to recast the building as a wellness center.
Discussions led to an agreement to work together, as well as a series of decisions. One early decision was that the group did not want to undertake a formal clinical research study approved by an Institutional Review Board, which would require steps that would slow down its process. “We wanted to make sure that we were optimizing this opportunity as it presented itself,” Hallberg said. Another decision was to take about three months of time to formulate a plan, including creating a logic model and a service blueprint, to ensure all the different participants could clearly articulate the plan and its goals to their stakeholders.
The resulting ten-month pilot gathered data from 47 people with diabetes. The pharmacy staff along with community health workers performed screenings and surveys, including measures of food insecurity, blood sugar and blood pressure, at the beginning, middle and end of the pilot. To deliver food, the pilot utilized a fleet of cars that the pharmacy already used daily to deliver medications to patients. Feed More provided the food boxes, which were delivered once a week to participants and provided both produce and shelf-stable food.
The results of the pilot were enough to generate interest from the Virginia state government as it contemplates various ways, such as 1115 waivers, to use Medicaid to support nutrition-led health initiatives. The pilot found an average decrease of 9.7% in blood sugar levels, as well as an average decrease in blood pressure from borderline high to normal among the participants. Self-reported screenings showed a 54% decrease in food insecurity and an 18.6% increase in access to nutritious food.
The results come at a time when governments are still trying to determine the value of nutrition-based interventions in healthcare and whether they should become reimbursable benefits. The pilot “added to the learnings and insights and excitement around the possibility for reimbursement for food-based supports,” Hallberg said. “This is definitely one of those pilots and outcomes that various stakeholders are pointing to.”
The pilot cost $95,000, primarily funded by United Healthcare. Part of the funding went toward transforming the former Jamaican restaurant into more of a wellness hub, where screenings and surveys took place. Money also went toward food, as well as incentives to get people to come into the hub and complete their health screenings.
Once the plan was agreed upon, the pilot was not difficult to pull off, Hallberg said. “The surprising part for me was how easy it was. Everyone had their role and everybody was responsible for their own things. It was very attainable,” she said. The only pivots came in accommodating people to make it easier for them to come into the wellness center to do their health screenings.
Looking forward, Feed More and the pharmacy are planning a seven-month pilot that will add medically tailored meals prepared in Feed More’s Community Kitchen. The pilot will focus on food-insecure patients with congestive heart failure who are being discharged from a local hospital.
Participants will receive eight weeks of support, including two weeks of meals and groceries, followed by six weeks of just groceries. The goal is to evaluate whether the support not only improves health outcomes and reduces food insecurity, but also decreases hospital readmissions.
Some might argue that food banks are stepping too far outside their normal scope when they get involved in activities like measuring blood sugar levels and hospital readmissions. In Hallberg’s view, the effort is worth the benefits to the community. “I think we have to care about the things that our stakeholders and funders care about,” she said, adding, “Ultimately, it’s about the whole health and well-being of the neighbor.” – Chris Costanzo
PHOTO, TOP: The Walnut Hill Wellness Hub, formerly a fast-food restaurant, played a role in Feed More’s Food is Medicine pilot.
Like what you’re reading?
Support Food Bank News