As more people recognize that food is integral to health, more hospital-based food pantries are turning up. In Chicago, one hospital has pioneered an “open-access” pantry model that it contends can be more beneficial to public health than other approaches.
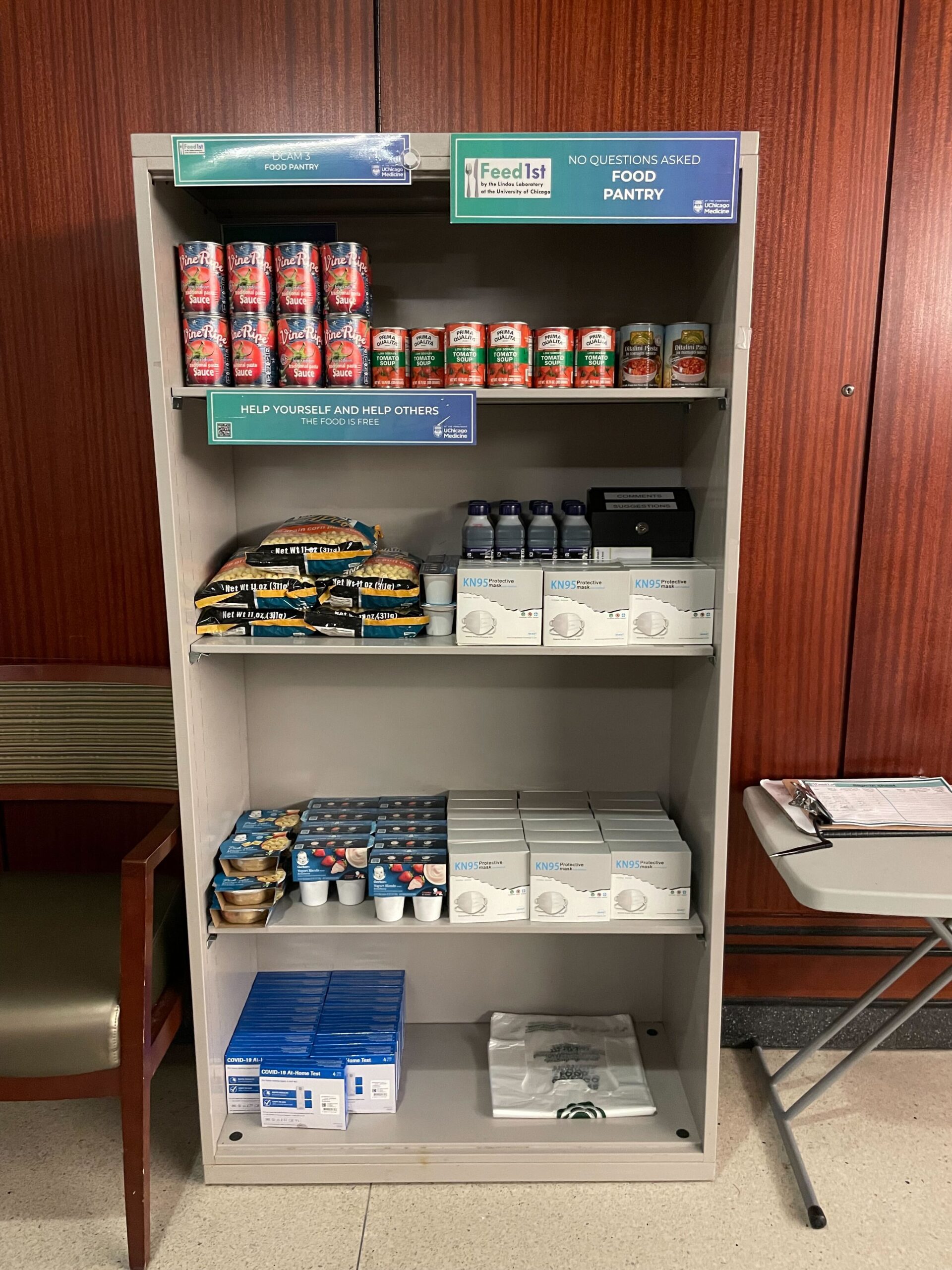
The Feed1st pantry at the University of Chicago Medical Center is actually a series of small pantries – 11 in all – spread throughout the facility. Located in family lounges, waiting areas, lobbies, and even the hospital cafeteria, the pantries emphasize easy access to food in stigma-free environments.

The self-service pantries invite people to take as much food as they need from the bookcase-like shelves, 24 hours a day, seven days a week. There is no data collection or other logistical hoops to jump through. A sign-up sheet is entirely voluntary.
The highly visible Feed1st pantries differ from standard hospital pantries, which may require a food prescription, or have limited hours, or operate from a single location. “We’re trying to get people healthy food without barriers,” said Mellissa Grana, Research Associate and Operations Lead for Feed1st.
A recent study pointed to the value of making pantry food easy to access in a hospital setting. For the six months between March and August 2020, Feed1st increased its distribution by 27% despite complications created by the pandemic, such as having to relocate some of the pantries. That stood in contrast to a more traditional food pantry at another hospital – which required an ID or referral, was not self-service, and had limited hours – and reported a decrease in food distributed during that time. Overall from March 2020 to November 2021, Feed1st increased its food distribution by 124% to nearly 43,000 pounds of food, compared to the same period two years prior.
The program began when a chaplain in the hospital, located on Chicago’s South Side, noticed that many families were skipping meals or eating poorly because they didn’t want to leave the facility and their loved ones. “What we were seeing was a lot of the children were hungry, and that obviously can contribute to why you’re in the hospital in the first place, whether it’s not eating enough or the quality of the food is not good enough to keep you healthy,” Grana said.
A central philosophy of Feed1st is that clients should not have to hand over personal data to get food. “We assume if you’re using the pantry and taking food, you need it,” explained Grana. “A lot of our community that we serve is food insecure, and going to the hospital and paying those medical bills is a big part of something that could keep you food insecure.”
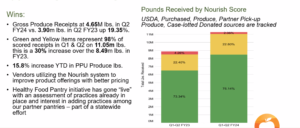
One of the challenges of this model is sourcing food. Because Feed1st does not collect information on who takes food from its pantries, it is ineligible for food from USDA programs. And though it is grandfathered in to receive food from its supplier, the Greater Chicago Food Depository, most food banks and grant providers are unable to offer that flexibility.
The program does its best to estimate how many people it serves in roundabout ways. Besides the voluntary sign-in sheets, the staff makes estimates based on the amount of food they set out. Soon, Grana said they will explore ways to get better data, such as observational studies to better estimate how many people who take food actually fill out the voluntary sheets.
But asking directly for a person’s name is out of the question, she said. “It’s very against the model.”
Unfortunately, the no-questions-asked approach has been a big barrier in being able to replicate the model with new partners. Feed1st has created a toolkit to help other hospitals build their own open-access pantry systems. So far, Johns Hopkins in Baltimore and Swedish Hospital, also in Chicago, have created pantry programs based on Feed1st’s learnings.
Ultimately, the team would like to create a nationwide Feed1st network that distributes food in medical settings in this stigma-free manner. “Our model is something we value very, very much, and we’d love to see more open access pantries that don’t ask any questions and that don’t create stigma or barriers to getting food,” Grana said.
Feed1st has found creative ways to stock its shelves. Since it can’t access produce through the USDA, the program has worked with a team of dietitians, nurses and nutritionists on its medical campus to source food from a rooftop garden on a parking garage that they voluntarily manage. Last year, the garden made it possible for Feed1st to distribute a ton of produce, including tomatoes, peppers, cabbage, kale and squash, alongside its shelf stable offerings.
Hospital staff are involved in Feed1st’s operations in other ways too. Medical students help store food and stock shelves, using the hospital’s tunnel system and local storage sites, and nurses and staff who work near each location serve as “champions,” by restocking and keeping things in order. The cafeteria staff have been welcoming of the pantry that is adjacent to their business, and said it has not affected sales.
“We believe we are successful because we were created for the community, by the community,” Grana said. Anyone is invited to participate by donating, volunteering, making suggestions or receiving a newsletter, and the pantry’s advisory board includes community members.
Being hospital-based also means that the pantries focus on healthy foods and dietary restrictions. There are no instant noodles, and Grana tries to offer whole grains as much as possible. She keeps the dietary needs of people who are sick in mind, such as offering almond milk for patients with diabetes who may not be allowed to have dairy.
Each location is designed to provide full meals, including proteins, vegetables, fruits, starches and grains. In the pantries in lounges, there are can openers, microwaves and ready to eat items. In places where people are more likely to take items home, there are grocery bags.
During the pandemic, Feed1st launched its first pantry inside a staff lounge, a recognition that many health care workers also struggle to pay their bills and find time to shop for food for their families. By making food available in a staff-only setting, Feed1st helps address the hesitation many of them have in taking food even though they have a job. “We want to assume that if you’re working full time, you have enough money to feed yourself and your family. However, that’s not always the case,” Grana said.
With its approach, Feed1st is seeking to provide not just access but agency. “The client experience we want people to have is that they’re in control of their lives,” she said, “in maybe situations where they feel really out of control.” – Ambreen Ali
Ambreen Ali writes the monthly Pantry Link column for Food Bank News. She is a widely published journalist and founding editor of Central Desi, a newsletter about New Jersey’s South Asian community.
CAPTION FOR PHOTO, TOP: One of Feed1st’s mini pantries is adjacent to the hospital’s cafeteria.
Like what you’re reading?
Support Food Bank News
This article was made possible by the readers who support Food Bank News, a national, editorially independent, nonprofit media organization. Food Bank News is not funded by any government agencies, nor is it part of a larger association or corporation. Your support helps ensure our continued solutions-oriented coverage of best practices in hunger relief. Thank you!
Connect with Us: